Smarter Management of Your Rx Benefits
Leading organizations depend on Remedy’s data intelligence and clinical insight to help reduce their drug spend and improve the management of members’ health.

The pharmacy landscape is complicated and often lacks transparency
Unchecked Rx prices
Pricing of prescription drugs is often inconsistent, and spending trends are accelerating at unprecedented rates, leaving employers and patients to cope with uncontrolled costs.
Opaque contracts
Vague language in PBM contracts can make it difficult for plan sponsors to interpret key terms.
Inadequate reporting
A typical PBM report shows high-level aggregate metrics that may not be either agnostic or actionable. Without an in-depth assessment of claims data, sponsors cannot evaluate opportunities at a granular level.
Lack of meaningful data analysis
Even when plan sponsors can see their claims data, they rarely have the time and means to interpret such a huge volume of complex information.
Fraud, waste and abuse
Low visibility into utilization patterns of prescription drugs can lead to mismanagement and, potentially, inappropriate usage.
Conflicts of interest
The distribution of medications in America from manufacturers to retail has many self-interested parties. Sponsors need a team whose only interest is to advocate on their behalf.
Unchecked Rx prices
Pricing of prescription drugs is often inconsistent, and spending trends are accelerating at unprecedented rates, leaving employers and patients to cope with uncontrolled costs.
Lack of meaningful data analysis
Even when plan sponsors can see their claims data, they rarely have the time and means to interpret such a huge volume of complex information.
Opaque contracts
Vague language in PBM contracts can make it difficult for plan sponsors to interpret key terms.
Fraud, waste and abuse
Low visibility into utilization patterns of prescription drugs can lead to mismanagement and, potentially, inappropriate usage.
Inadequate reporting
A typical PBM report shows high-level aggregate metrics that may not be either agnostic or actionable. Without an in-depth assessment of claims data, sponsors cannot evaluate opportunities at a granular level.
Conflicts of interest
The distribution of medications in America from manufacturers to retail has many self-interested parties. Sponsors need a team whose only interest is to advocate on their behalf.

A new standard for the management of prescription benefits
Get unbiased industry recommendations backed by agnostic data insights.
Remedy’s Reach
3M+
Claims Analyzed Each Month
$700M+
Saved Annually
3.3M+
Members Under Service
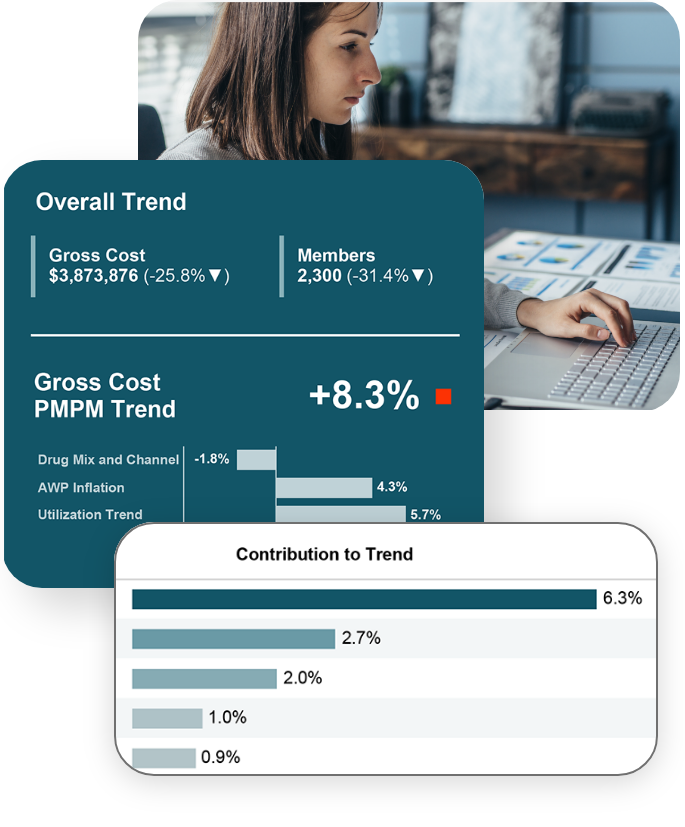
PharmaLogic®
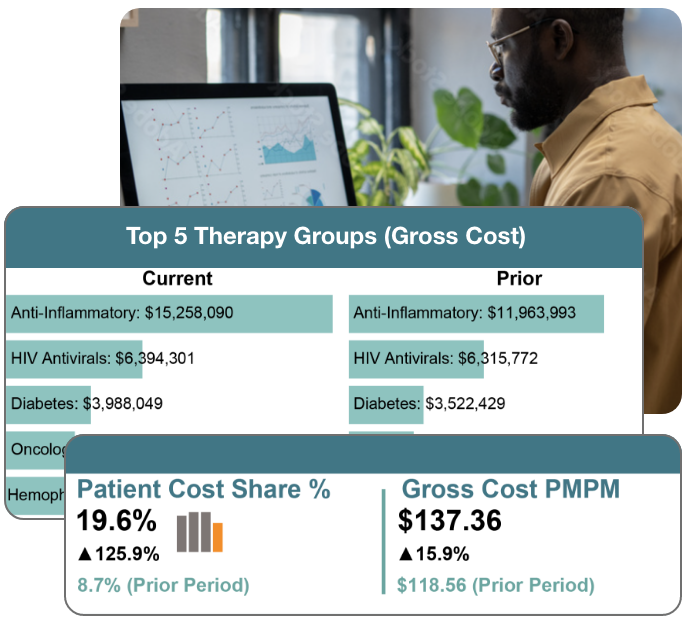
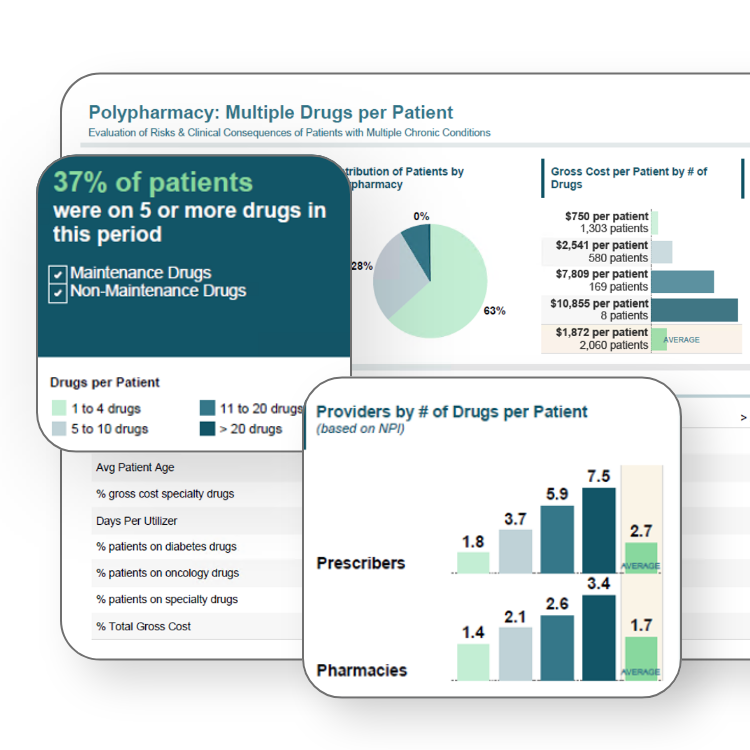
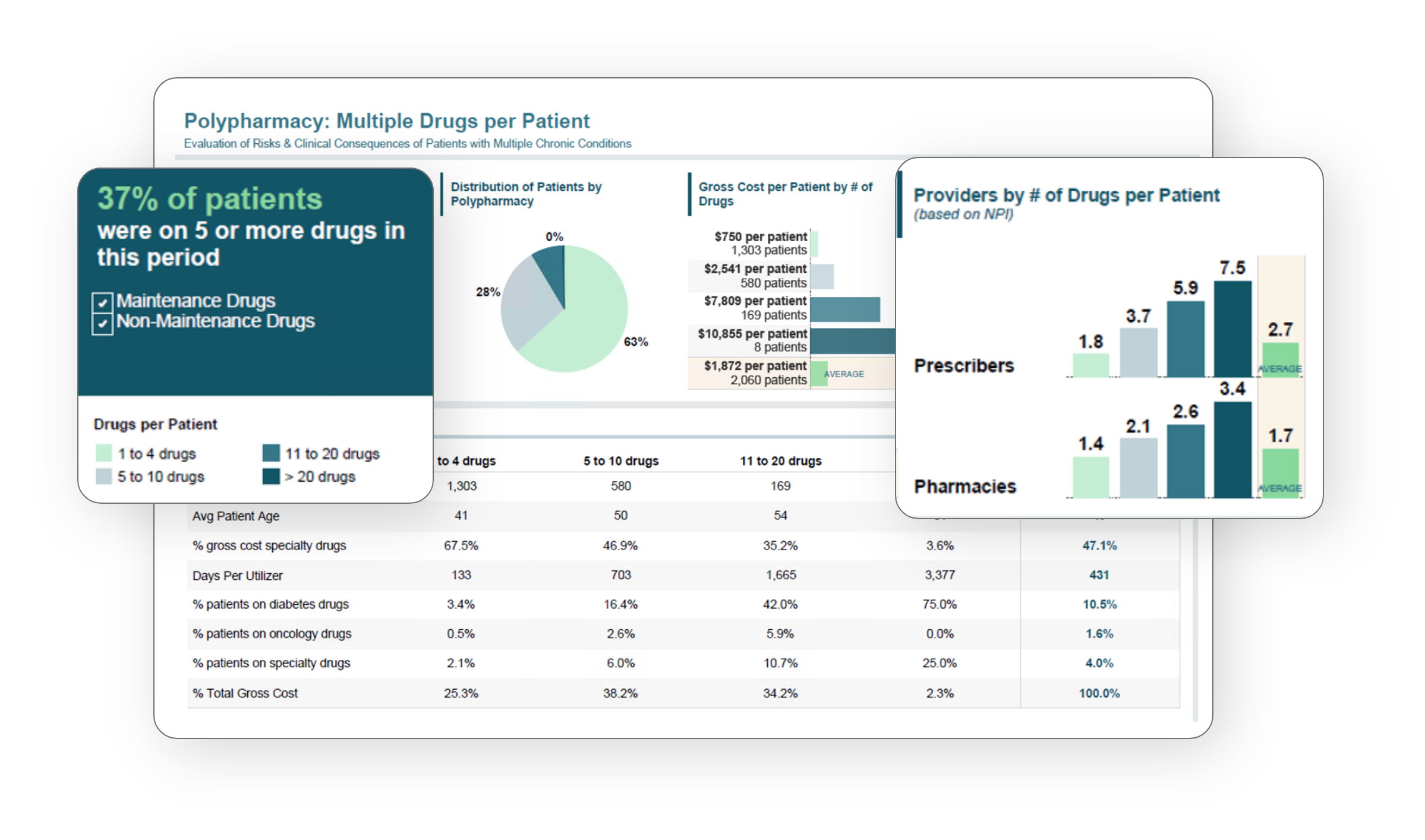
Remedy’s state-of-the-art technology provides unrivaled analytics. By processing data on a granular level, PharmaLogic® identifies both financial inefficiencies and clinical opportunities in your pharmacy benefits. With frequent monitoring throughout the year of drug utilization, claims adjudication and adherence to contract terms, PharmaLogic® is the data-driven blueprint for smarter management.
Full-service Rx consulting
Payers get next-level support with Remedy’s data intelligence and industry guidance.
Market Checks
Secure the most competitive drug pricing through Remedy-renegotiated terms so you maximize your Rx benefits each year.
Learn More >>
PharmaLogic®
Robust data analytics platform that identifies cost/utilization drivers and evaluates plan performance with frequent monitoring of Rx claims
Learn More >>
RFPs
Asking hard questions and insisting on full answers lead to thorough proposals that reveal a PBM’s true value.
Learn More >>
Consulting
Seasoned PBM professionals, actuaries, clinicians and data engineers deliver customized solutions that help meet your goals.
Learn More >>
Clinical Insights
Stay ahead of industry trends and understand the impact of market events and how they affect your members.
Learn More >>
Auditing
Remedy utilizes PharmaLogic® to conduct an in-depth review of every claim to verify compliance to pricing and contract criteria as outlined in a customer’s PBM agreement.
Learn More >>
To make prescription drugs more affordable and accessible for payers and patients for optimal health
Remedy's Clients